
Power your paddle sports with three great exercises

On the Gulf Coast of Florida where I live, the telltale sign of summer is not an influx of beachcombers, afternoon storms that arrive exactly at 2 p.m., or the first hurricane warning, but the appearance of hundreds of paddleboarders dotting the inlet waters.
From afar, paddleboarding looks almost spiritual — people standing on nearly invisible boards and gliding across the surface as if walking on water.
But this popular water sport offers a serious workout, just as kayaking and canoeing do. While floating along and casually dipping a paddle in the water may look effortless, much goes on beneath the surface, so to speak.
As warm weather beckons and paddle season arrives, it pays to get key muscles in shape before heading out on the water.
Tuning up muscles: Focus on core, back, arms, and shoulders
“Paddling a kayak, canoe, or paddleboard relies on muscles that we likely haven’t used much during winter,” says Kathleen Salas, a physical therapist with Spaulding Adaptive Sports Centers at Harvard-affiliated Spaulding Rehabilitation Network. “Even if you regularly weight train, the continuous and repetitive motions involved in paddling require endurance and control of specific muscles that need to be properly stretched and strengthened.”
While paddling can be a whole-body effort (even your legs contribute), three areas do the most work and thus need the most conditioning: the core, back, and arms and shoulders.
- Core. Your core comprises several muscles, but the main ones for paddling include the rectus abdominis (that famed “six-pack”) and the obliques, located on the side and front of your abdomen. The core acts as the epicenter around which every movement revolves — from twisting to bending to stabilizing your trunk to generate power.
- Back: Paddling engages most of the back muscles, but the ones that carry the most load are the latissimus dorsi muscles, also known as the lats, and the erector spinae. The lats are the large V-shaped muscles that connect your arms to your vertebral column. They help protect and stabilize your spine while providing shoulder and back strength. The erector spinae, a group of muscles that runs the length of the spine on the left and right, helps with rotation.
- Arms and shoulders: Every paddle stroke engages the muscles in your arms (biceps) and the top of your shoulder (deltoids).
Many exercises specifically target these muscles, but here are three that can work multiple paddling muscles in one move. Add them to your workouts to help you get ready for paddling season. If you haven’t done these exercises before, try the first two without weights until you can do the movement smoothly and with good form.
Three great exercises to prep for paddling
Wood chop


Muscles worked: Deltoids, obliques, rectus abdominis, erector spinae
Reps: 8–12 on each side
Sets: 1–3
Rest: 30–90 seconds between sets
Starting position: Stand with your feet about shoulder-width apart and hold a dumbbell with both hands. Hinge forward at your hips and bend your knees to sit back into a slight squat. Rotate your torso to the right and extend your arms to hold the dumbbell on the outside of your right knee.
Movement: Straighten your legs to stand up as you rotate your torso to the left and raise the weight diagonally across your body and up to the left, above your shoulder, while keeping your arms extended. In a chopping motion, slowly bring the dumbbell down and across your body toward the outside of your right knee. This is one rep. Finish all reps, then repeat on the other side. This completes one set.
Tips and techniques:
- Keep your spine neutral and your shoulders down and back
- Reach only as far as is comfortable.
- Keep your knees no farther forward than your toes when you squat.
Make it easier: Do the exercise without a dumbbell.
Make it harder: Use a heavier dumbbell.
Bent-over row


Muscles worked: Latissimus dorsi, deltoids, biceps
Reps: 8–12
Sets: 1–3
Rest: 30–90 seconds between sets
Starting position: Stand with a weight in your left hand and a bench or sturdy chair on your right side. Place your right hand and knee on the bench or chair seat. Let your left arm hang directly under your left shoulder, fully extended toward the floor. Your spine should be neutral, and your shoulders and hips squared.
Movement: Squeeze your shoulder blades together, then bend your elbow to slowly lift the weight toward your ribs. Return to the starting position. Finish all reps, then repeat with the opposite arm. This completes one set.
Tips and techniques:
- Keep your shoulders squared throughout.
- Keep your elbow close to your side as you lift the weight.
- Keep your head in line with your spine.
Make it easier: Use a lighter weight.
Make it harder: Use a heavier weight.
Superman


Muscles worked: Deltoids, latissimus dorsi, erector spinae
Reps: 8–12
Sets: 1–3
Rest: 30–90 seconds between sets
Starting position: Lie face down on the floor with your arms extended, palms down, and legs extended.
Movement: Simultaneously lift your arms, head, chest, and legs off the floor as high as is comfortable. Hold. Return to the starting position.
Tips and techniques:
- Tighten your buttocks before lifting.
- Don’t look up.
- Keep your shoulders down, away from your ears.
Make it easier: Lift your right arm and left leg while keeping the opposite arm and leg on the floor. Switch sides with each rep.
Make it harder: Hold in the “up” position for three to five seconds before lowering.
About the Author

Matthew Solan, Executive Editor, Harvard Men's Health Watch
Matthew Solan is the executive editor of Harvard Men’s Health Watch. He previously served as executive editor for UCLA Health’s Healthy Years and as a contributor to Duke Medicine’s Health News and Weill Cornell Medical College’s … See Full Bio View all posts by Matthew Solan
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

How healthy is sugar alcohol?

If you are trying to cut back on added sugar — and you should, because excess sugar increases risks for obesity, diabetes, and heart disease — you might be tempted by products advertised as low sugar, no sugar, or sugar-free.
Many contain familiar low-calorie sugar substitutes like aspartame or sucralose instead of sugar. And as you’re reading labels, you also may run across another ingredient: sugar alcohol, which is used in products like sugar-free cookies, candies, ice cream, beverages, and chewing gums. Are any of these sweeteners a better choice nutritionally? Dr. Frank Hu, professor of nutrition and epidemiology with the Harvard T.H. Chan School of Public Health, weighs in below.
Are low-calorie or no-calorie sweeteners any healthier than natural sugar?
Also known as artificial sweeteners or sugar substitutes, the list of low-calorie and no-calorie sweeteners you may see on product nutrition labels includes acesulfame-K, saccharin, sucralose, neotame, and advantame. These have a higher sweetness intensity per gram than natural sugar.
So far research on them is mixed, although some observational studies have found that beverages containing low-calorie sweeteners are associated with a higher risk for diabetes and weight gain.
What exactly are sugar alcohols and how can you spot them?
Sugar alcohols may have the most misleading name, as they are neither sugar nor alcohol, according to Dr. Hu. “They are a type of carbohydrate derived from fruits and vegetables, although most commercial sugar alcohols are synthetically produced.”
You can usually spot many sugar alcohols on ingredient lists by “-ol” at the ends of their names. Examples include sorbitol, xylitol, lactitol, mannitol, erythritol, and maltitol.
Are sugar alcohols any healthier than other sugar substitutes or natural sugar?
Here is a look at the pros and cons.
The upside of sugar alcohols
Sugar alcohols reside in the sweet spot between natural sugar and low-calorie sweeteners. They are not as overly sweet as sweeteners and don’t add too many extra calories like sugar.
“Sugar alcohols are about 40% to 80% as sweet as natural sugar, whereas artificial sweeteners like aspartame are about 200 times sweeter,” says Dr. Hu. “And they have about 25% to 75% fewer calories per gram than sugar.”
Another upside of sugar alcohols is that they break down slowly in the gut. Hence, your body only absorbs part of their overall carbohydrates. “This keeps your blood sugar and insulin levels from spiking as they do with sugar,” says Dr. Hu. “That makes them a useful sugar substitute for people with diabetes.”
The downside of sugar alcohols
The main downside to sugar alcohols is this: when taken in high amounts they can cause gastrointestinal (GI) problems, such as abdominal pain, diarrhea, or loose stools.
Because sugar alcohols are slowly digested, they have more time to feed bacteria in the gut, which can lead to fermentation and produce excess gas. Their slow digestion also can pull extra water into the colon and cause a laxative effect.
People’s tolerance for sugar alcohols depends on many factors, including body weight, health conditions, and the amount and types of sugar alcohols. “Individual differences in digestion and metabolism, gut microbiome composition, and dietary habits can also make a difference,” says Dr. Hu. “For these reasons, we recommend introducing sugar alcohols into your diet gradually and observing how your body responds.”
For people who experience GI symptoms caused by sugar alcohols, Dr. Hu says cutting back on the amount of foods and drinks made with them often can correct the problem. “Sugar alcohols are commonly found in sugar-free or low-carb products, so pay attention to food labels” he says. “Because different sugar alcohols can have different effects, it might be useful to identify specific types of sugar alcohols that cause GI side effects.”
Do sugar alcohols have health risks?
Possible long-term health risks of sugar alcohol are still being explored. A 2023 observational study found a link between using erythritol as an added sweetener and cardiovascular disease events, such as stroke and heart attack, in people with heart disease or who had risk factors like diabetes and high blood pressure. However, these findings have not been confirmed in subsequent studies.
“Sugar alcohols offer a healthier alternative to sugar because of their lower calorie content and reduced glycemic response, which is the effect food has on blood sugar levels,” says Dr. Hu. “But they also have potential drawbacks, especially for those with sensitive digestive systems, so it’s best to consume them in moderation as part of an overall healthy eating pattern.”
About the Author

Matthew Solan, Executive Editor, Harvard Men's Health Watch
Matthew Solan is the executive editor of Harvard Men’s Health Watch. He previously served as executive editor for UCLA Health’s Healthy Years and as a contributor to Duke Medicine’s Health News and Weill Cornell Medical College’s … See Full Bio View all posts by Matthew Solan
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD
Salmonella is sneaky: Watch out
Pop quiz: what is Salmonella? If you’ve ever had a run-in with this bacteria, you know it can cause a food-borne illness called salmonellosis, a form of food poisoning. But you may not know that Salmonella bacteria sicken an estimated 1.35 million people and hospitalize 26,500 every year in the United States. What’s more, it kills more total people than any other type of food poisoning.
And Salmonella bacteria can be sneaky — not only by triggering unusual complications, but infecting people in startling ways, says Dr. Elizabeth Hohmann, an infectious disease specialist at Massachusetts General Hospital. One patient she treated showed up with an abdominal aortic aneurysm — a dangerous bulge in the lower section of the body’s largest artery — that looked infected. Testing revealed a culprit some would find surprising: Salmonella.
“It’s just an interesting organism and it can be kind of scary,” she says.
How do people get infected by Salmonella?
Many of the foods Salmonella bacteria lurk in are raw or undercooked. Breaded raw chicken products like nuggets and chicken Kiev are one way it may reach your table. But a variety of foods have been implicated — including organic basil, cantaloupes, ground beef, nut butters, raw cookie dough, eggs, raw or unpasteurized milk, and flour.
Even small pets such as turtles and frogs, along with dog food, have contributed to Salmonella outbreaks in recent years.
You can also become infected by handling contaminated food and spreading the bacteria from your hands to your mouth. Additionally, you can spread it to others on your hands or even on your clothes without becoming sick yourself.
“It’s a bug that’s carried in stool and animal feces and is also present in the environment,” Dr. Hohmann says. “So it can set up shop in lots of different inanimate objects, soils, and machinery, especially in moist environments.”
What symptoms can Salmonella cause?
Most of the time, Salmonella infection leads to gastroenteritis, usually causing just an upset stomach, abdominal cramps, and diarrhea. These symptoms can start as soon as six hours after ingesting the bacteria. Typically, symptoms resolve on their own within two to three days.
Some people have such mild symptoms they’re barely noticeable. “The classic case might be a college student who eats a burrito from a sketchy place, gets sick for a couple of days, gets better, and doesn’t think anything of it,” says Dr. Hohmann.
Sometimes symptoms are more serious, such as severe abdominal cramping and bloody diarrhea, or unexplained high fever and marked fatigue. These symptoms require a call to your doctor.
How is salmonellosis treated?
Most people will get better on their own without any medicines. Replacing lost fluids by sipping water or electrolyte drinks to avoid dehydration will help.
Call a doctor if you have
- diarrhea and a fever higher than 102° F
- diarrhea that doesn’t improve after three days
- bloody stools
- vomiting so severe it prevents you from keeping liquids down.
Treating the infection with medicine comes with an annoying paradox, Dr. Hohmann says. If doctors decide to prescribe antibiotics, the person taking the medicine may shed the organism for longer than if they were never treated. “Then that person may have the opportunity — either through poor personal hygiene, sex, or working as a food worker — to spread it to others,” she explains. “It’s challenging.”
What complications can Salmonella lead to?
Some people get sicker with salmonellosis than others, with seemingly no rhyme or reason. But certain folks are especially vulnerable to serious infection, including:
- adults 65 and older
- pregnant women
- children under 5
- people whose immune systems are weakened by diseases (such as cancer) or treatments (such as immunosuppressing drugs).
A small percentage of those infected can have Salmonella in their blood, which can spread the infection to other parts of the body such as the urinary tract, bones, joints, or central nervous system (brain and spinal fluid).
And, like Dr. Hohmann’s patient with the abdominal aortic aneurysm, on rare occasions Salmonella can lead to unusual blood vessel complications in people who already have atherosclerosis, blockage of the arteries caused by plaque buildup.
“It’s not that common,” she says. “Many physicians are aware of it, so they take special care if Salmonella is found in a person with vascular disease.”
What steps can you take to avoid Salmonella?
While new USDA rules that take effect in 2025 may help fuel recalls of certain foods, we all can take steps to avoid the food poisoning, illness, and hospitalizations that Salmonella exposure can cause.
Dr. Hohmann and the CDC suggest these strategies:
- Using hot water and soap, wash cutting boards or plates on which you cut into raw foods — including vegetables and fruit — before using those surfaces for other purposes. If possible, use separate cutting boards for produce, meat, and fish.
- Refrigerate or freeze foods that are perishable, prepared, or left over within two hours to thwart salmonella growth.
- Always wash hands well with soap and water before preparing food and after contact with animals, using the toilet, or changing diapers.
- If you have a sick pet, take extra care handling its feces and wash your hands thoroughly afterward.
Take additional steps to help more vulnerable people stay healthy:
- Don’t let young children touch high-risk animals, such as turtles, frogs, chickens, or ducks. “And if you’re taking young children to a petting zoo, they should not be petting animals unless you can disinfect their hands immediately afterward,” she says.
- Older adults and those with compromised immune systems should take extra care to wash and cook foods thoroughly.
- People who have had a transplant (such as a kidney transplant) should not keep reptiles or amphibians as pets.
“You hate to make people paranoid, so that we’re washing our lettuce leaves with soap, but it’s worth thinking about these things, particularly if you have people in your household who are susceptible — which is an increasing number of people,” Dr. Hohmann says.
About the Author
Maureen Salamon, Executive Editor, Harvard Women's Health Watch
Maureen Salamon is executive editor of Harvard Women’s Health Watch. She began her career as a newspaper reporter and later covered health and medicine for a wide variety of websites, magazines, and hospitals. Her work has … See Full Bio View all posts by Maureen Salamon
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

New urine test may help some men with elevated PSA avoid biopsy

When a prostate-specific antigen (PSA) blood test produces an abnormal result, the next step is usually a prostate biopsy. A biopsy can confirm or rule out a cancer diagnosis, but it also has certain drawbacks. Prostate biopsies are invasive procedures with potential side effects, and they often detect low-grade, slow-growing tumors that may not need immediate treatment — or any treatment at all.
Researchers are exploring various strategies for avoiding unnecessary biopsies. Specialized magnetic resonance imaging (MRI) scans, for instance, can be useful for predicting if a man’s tumor is likely to spread. A blood test called the Prostate Health Index (PHI) measures various forms of PSA, and can help doctors determine if a biopsy is needed.
In April, researchers at the University of Michigan published results with a test that screens for prostate cancer in urine samples. Called the MyProstateScore 2.0 (MPS2) test, it looks for 18 different genes associated with high-grade tumors. “If you’re negative on this test, it’s almost certain that you don’t have aggressive prostate cancer,” said Dr. Arul Chinnaiyan, a professor of pathology and urology at the University, in a press release.
Gathering data and further testing
To create the test, Dr. Chinnaiyan and his colleagues first turned to publicly-available databases containing over 58,000 prostate cancer-associated genes. From that initial pool, they narrowed down to 54 genes that are uniquely overexpressed in cancers classified as Grade Group 2 (GG2) or higher. The Grade Group system ranks prostate cancers from GG1 (the least dangerous) to GG5 (the most dangerous).
The team tested those 54 genes against archived urine samples from 761 men with elevated PSA who were scheduled for biopsy. This effort yielded 18 genes that consistently correlated with high-grade cancer in the biopsy specimens. These genes now make up MPS2.
Then the team validated the test by performing MPS2 testing on over 800 archived urine samples collected by a national prostate cancer research consortium. Other researchers affiliated with that consortium assessed the new urine test’s results against patient records.
Interpreting the results
Study findings showed that MPS2 correctly identified 95% of the GG2 prostate cancers and 99% of cancers that were GG3 or higher. Test accuracy was further improved by incorporating estimates of the prostate’s size (or volume, as it’s also called).
According to the team’s calculations, use of the MPS2 would have reduced unnecessary biopsies by 37%. If volume was included in the measure, then 41% of biopsies would have been avoided. By comparison, just 26% of biopsies would have been avoided with the PHI.
Dr. Chinnaiyan and his co-authors emphasize that ruling out high-grade cancer with a urine test offers some advantages over MRI. The specialized multi-parametric MRI scans needed to assess high-grade cancer in men with elevated PSA aren’t always available in community settings, for instance. Moreover, the interpretation of mpMRI results can vary from one radiologist to another. Importantly, the MPS2 can be updated over time as new prostate-cancer genes are identified.
Commentary
Dr. Boris Gershman, a urologist at Harvard-affiliated Beth Israel Deaconess Medical Center in Boston, and a member of the advisory and editorial board for the Harvard Medical School Guide to Prostate Diseases, described the new study results as promising. “It does appear that the performance of the 18-gene urine test is better than PSA alone,” he says.
But Dr. Gershman adds that it will be important to consider how such a test will fit into the current two-stage approach for PSA screening, which entails prostate MRI when the PSA is abnormal. Where MRI delivers a yes/no result (meaning lesions that look suspicious for cancer are either present or not), the MPS2 provides numerical risk estimates ranging between 0% and 100%. “The challenge with clinical implementation of a continuous risk score is where to draw the line for biopsy,” Dr. Gershman says.
“This research is very encouraging, since many men in rural areas may not have access to prostate MRI machines or the added sophistication that is needed in interpreting these MRI scans,” says Dr. Marc Garnick, the Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center. “A widely available urine test may eventually help provide more precision in determining who should undergo a prostate biopsy, and may also help to assess the probability that a cancer is clinically significant and in need of treatment.”
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt
About the Reviewer
Marc B. Garnick, MD, Editor in Chief, Harvard Medical School Annual Report on Prostate Diseases; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Marc B. Garnick is an internationally renowned expert in medical oncology and urologic cancer. A clinical professor of medicine at Harvard Medical School, he also maintains an active clinical practice at Beth Israel Deaconess Medical … See Full Bio View all posts by Marc B. Garnick, MD

Why play? Early games build bonds and brain

Want your child to grow up healthy, happy, smart, capable, and resilient? Play with them. Infants and toddlers thrive on playful games that change as they grow.
Why does play matter during the first few years of life?
More than a million new nerve connections are made in the brain in the first few years of life. And pruning of these neural connections makes them more efficient. These processes literally build the brain and help guide how it functions for the rest of that child’s life. While biology — particularly genetics — affects this, so does a child’s environment and experiences.
Babies and children thrive with responsive caregiving. Serve and return, a term used by the Harvard Center on the Developing Child, describes this well: back-and-forth interactions, in which the child and caregiver react to and interact with each other in a loving, nurturing way, are the building blocks of a healthy brain and a happy child, who will have a better chance of growing into a healthy, happy, competent, and successful adult.
Play is one of the best ways to do responsive caregiving. To maximize the benefits of play:
- Bring your full attention. Put the phone down, don’t multitask.
- Be reciprocal. That’s the “serve and return” part. Even little babies can interact with their caregivers, and that’s what you want to encourage. It doesn’t have to be reciprocal in an equal way — you might be talking in sentences while your baby is just smiling or cooing — but the idea is to build responsiveness into the play.
- Be attuned to developmental stages. That way your child can fully engage — and you can encourage their development as well.
Great games to play with infants: 6 to 9 months
The Center for the Developing Child has some great ideas and handouts for parents about specific games to play with their children at different ages.
6-month-olds and 9-month-olds are learning imitation and other building blocks of language. They are also starting to learn movement and explore the world around them.
Here are some play ideas for this age group:
- Play peek-a-boo or patty-cake.
- Play games of hiding toys under a blanket or another toy, and then “find” them, or let the baby find them.
- Have back-and-forth conversations. The baby’s contribution might just be a “ma” or “ba” sound. You can make the same sound back, or pretend that your baby is saying something (“You don’t say! Really? Tell me more!”).
- Play imitation games: if your baby sticks out their tongue, you do it too, for example. Older babies will start to be able to imitate things like clapping or banging, and love when grownups do that with them.
- Sing songs that involve movement, like “Itsy Bitsy Spider” or “Trot, Trot to Boston” with words and motions.
- Play simple games with objects, like putting toys into a bucket and taking them out, or dropping them and saying “boom!”
Great games to play with toddlers
Between 12 months and 18 months, young toddlers are gaining more language and movement skills, and love to imitate. You can:
- Play with blocks, building simple things and knocking them down together.
- Do imaginative play with dolls or stuffed animals, or pretend phone calls.
- Use pillows and blankets to build little forts and places to climb and play.
- Play some rudimentary hide-and-seek, like hiding yourself under a blanket next to the baby.
- Continue singing songs that involve movement and interaction, like “If You’re Happy And You Know It.”
- Go on outings and explore the world together. Even just going to the grocery store can be an adventure for a baby. Narrate everything. Don’t worry about using words your baby doesn’t understand; eventually they will, and hearing lots of different words is good for them.
Older toddlers, who are 2 or 3 years old, are able to do more complicated versions of these games. They can do matching, sorting, and counting games, as well as imitation and movement games like “follow the leader” (you can get quite creative and silly with that one).
As much as you can, give yourself over to play and have fun. Work and chores can wait, or you can actually involve young children in chores, making that more fun for both of you. Checking social media can definitely wait.
Playing with your child is an investment in your child’s future — and a great way to build your relationship and make both of you happy.
About the Author

Claire McCarthy, MD, Senior Faculty Editor, Harvard Health Publishing
Claire McCarthy, MD, is a primary care pediatrician at Boston Children’s Hospital, and an assistant professor of pediatrics at Harvard Medical School. In addition to being a senior faculty editor for Harvard Health Publishing, Dr. McCarthy … See Full Bio View all posts by Claire McCarthy, MD
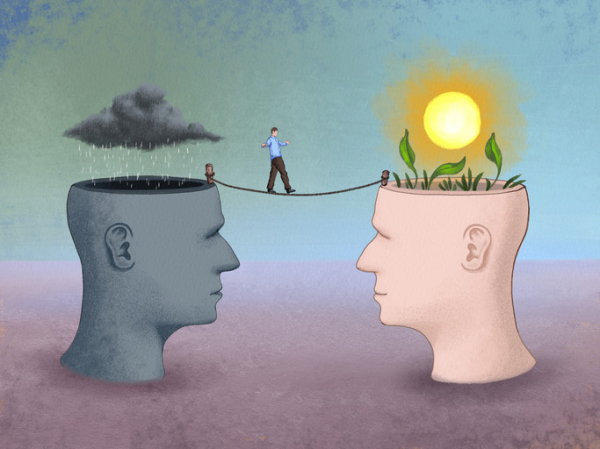
What is cognitive behavioral therapy?
Cognitive behavioral therapy (CBT) teaches people to challenge negative thought patterns and turn less often to unhelpful behaviors. These strategies can improve your mood and the way you respond to challenging situations: a flat tire, looming deadlines, family life ups and downs.
Yet there’s much more depth and nuance to this well-researched form of psychotherapy. It has proven effective for treating anxiety, depression, and other mental health conditions. Tailored versions of CBT can also help people cope with insomnia, chronic pain, and other nonpsychiatric conditions. And it can help in managing difficult life experiences, such as divorce or relationship problems.
What are the key components of CBT?
One important aspect of CBT relates to perspective, says psychologist Jennifer Burbridge, assistant director of the Cognitive Behavioral Therapy Program at Harvard-affiliated Massachusetts General Hospital.
“Therapists who practice CBT don’t see the problems or symptoms people describe as having one single cause, but rather as a combination of underlying causes,” she says. These include
- biological or genetic factors
- psychological issues (your thoughts, physical sensations, and behaviors)
- social factors (your environment and relationships).
Each of these factors contributes to — and helps maintain — the troublesome issues that might prompt you to seek therapy, she explains.
How does CBT describe our emotions?
Our emotions have three components: thoughts, physical sensations, and behaviors.
“Thoughts are what we say to ourselves, or 'self-talk,'” says Burbridge. Physical sensations are what we observe in our bodies when we experience an emotional situation: for example, when your heart rate rises in stressful circumstances. Behaviors are simply the things you do — or do not do. For instance, anxiety might prevent you from attending a social event.
All three components are interrelated and influence one another. That’s why CBT helps people to develop skills in each of them. “Think of it as a wellness class for your emotional health,” says Burbridge.
How long does CBT last?
CBT is a goal-oriented, short-term therapy. Typically it involves weekly, 50-minute sessions over 12 to 16 weeks. Intensive CBT may condense this schedule into sessions every weekday over one to three weeks.
Is CBT collaborative?
“When I first meet with someone, I’ll listen to what’s going on with them and start thinking about different strategies they might try,” Burbridge says. But CBT is a collaborative process that involves homework on the patient’s part.
What might that mean for you? Often, a first assignment involves self-monitoring, noting whether there are certain things, events, or times of day that trigger your symptoms. Future sessions focus on fine-tuning approaches to elicit helpful, adaptive self-talk, and problem-solving any obstacles that might prevent progress.
Certain thinking patterns are often associated with anxiety or depression, says Burbridge. Therapists help people recognize these patterns and then work with patients to find broader, more flexible ways to cope with difficult situations.
“We’re cognitive creatures with big frontal lobes that help us analyze situations and solve problems. That’s useful in some situations. But at other times, when you’re trying to manage your emotions, it may be better to pause and acknowledge and accept your discomfort,” says Burbridge.
Which CBT tools and strategies can help?
That particular skill — paying attention in the present moment without judgement, or mindfulness — is a common CBT tool. Another strategy that’s helpful for anxiety, known as exposure or desensitization, involves facing your fears directly.
“People avoid things that make them nervous or scared, which reinforces the fear,” says Burbridge. With small steps, you gradually expose yourself to the scary situation. Each step provides learning opportunities — for example, maybe you realize that the situation wasn’t as scary as you though it would be.
By trying new things instead of avoiding them, you begin to change your thought patterns. These more adaptive thinking patterns then make it more likely you will try new or challenging experiences in the future, thereby increasing your self-confidence.
How does CBT work?
Brain imaging research suggests conditions like depression or anxiety change patterns of activity in certain parts of the brain. One way CBT may help address this is by modifying nerve pathways involved in fear responses, or by establishing new connections between key parts of the brain.
A 2022 review focused on 13 brain imaging studies of people treated with CBT. The analysis suggested CBT may alter activity in the prefrontal cortex (often called the “personality center”) and the precuneus (which is involved in memory, integrating perceptions of the environment, mental imagery, and pain response).
Who might benefit from CBT?
CBT is appropriate for people of all different ages. This can range from children as young as 3 years — in tandem with parents or caregivers — to octogenarians. In addition to treating anxiety and depression, CBT is also effective for
- eating disorders
- substance abuse
- personality disorders
- attention deficit hyperactivity disorder (ADHD)
- obsessive compulsive disorder (OCD).
Additional evidence shows CBT may help people with different health issues, including irritable bowel syndrome, chronic fatigue syndrome, fibromyalgia, insomnia, migraines, and other chronic pain conditions. The therapy may also benefit people with cancer, epilepsy, HIV, diabetes, and heart disease.
“Many medical conditions can limit your activities. CBT can help you adjust to your diagnosis, cope with the new challenges, and still live a meaningful life, despite the limitations,” says Burbridge.
About the Author

Julie Corliss, Executive Editor, Harvard Heart Letter
Julie Corliss is the executive editor of the Harvard Heart Letter. Before working at Harvard, she was a medical writer and editor at HealthNews, a consumer newsletter affiliated with The New England Journal of Medicine. She … See Full Bio View all posts by Julie Corliss
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

Moving from couch to 5K

Need a little motivation and structure to ramp up your walking routine? Want to wake up your workouts but not quite ready for a mud run? Consider trying a couch-to-5K program.
Dr. Adam Tenforde, medical director of the Spaulding National Running Center at Harvard-affiliated Spaulding Rehabilitation Network and a sports medicine physician at Mass General Brigham Sports Medicine, shares tips on what to know and do before lacing up your sneakers.
What is a couch-to-5K program?
These free or low-cost coaching plans are designed to help would-be runners train for a 5-kilometer race, which is about 3.1 miles. The programs are available online, or as apps or podcasts. They typically feature timed walking and running intervals that gradually phase out the walking over a period of about nine weeks.
Why try a couch-to-5K program?
“One purpose of a couch-to-5K program is to give you time to acclimate and start to enjoy the benefits of running and the sense of accomplishment of completing a distance safely,” says Dr. Tenforde. Running provides many cardiovascular benefits, such as lower blood pressure and a reduced cholesterol level, as well as an enhanced sense of well-being, he adds.
What’s more, adding even short bursts of running or other vigorous physical activity to a workout — a practice known as high-intensity interval training or HIIT — appears to help improve mental health, according to a study that pooled findings from 58 randomized trials of HIIT.
Are you ready to tackle a couch-to-5K?
Even though the couch-to-5K programs sound as though they’re geared for completely sedentary couch potatoes, that’s not necessarily true, Dr. Tenforde cautions. These programs often assume you can walk continuously for 30 minutes, which doesn’t apply to everyone.
For some people, an even easier, more gradual training regimen may be more appropriate. Also, keep in mind that you don’t have to run to do a 5K. Many of these races also encourage walkers to participate as well. You’ll still reap the other rewards from committing to a race, such as being more challenged and motivated — and possibly more connected to your community. Many charitable “fun runs” benefit local schools or needy families. Some are in memory of people affected by illness or tragedy. Visit Running in the USA to find 5K races near you.
What to do before you start
If you’re planning to walk or run your first 5K, get your doctor’s approval before you start training. That’s especially important if you have heart disease or are at risk for it.
Comfortable walking or running shoes are a wise investment. Shoes that are too old or too tight in the toe box can cause or aggravate a bunion, a bony bump at the outer base of the big toe. Despite suggestions that people with flat feet or high arches need specific types of shoes, studies have found that neutral shoes (designed for average feet) work well for almost everyone. Walk or jog around the store when you try them on to make sure they feel good and fit properly.
You don’t need to buy special clothes; regular sweat pants or comfortable shorts and a t-shirt will suffice. Women should consider getting a supportive sports bra, however.
Go slow and steady when training
- Always include a warm-up and cool-down — a few minutes of slow walking or jogging — with every exercise session.
- If you haven’t been exercising regularly, start by walking just five or 10 minutes a day, three days a week. Or, if you’re already a regular walker, add some short stints of jogging to each walking session.
- Gradually add minutes and days over the following four to six weeks.
- Once you’re up to 30 minutes a day, check how far you’re traveling. Keep increasing your distance every week until you reach 5 kilometers. Then slowly phase in more jogging and less walking over your route if you like.
Remember that you can always repeat a week. You’re less likely to sustain an injury if you make slow, steady progress. Pay close attention to your body and don’t push yourself too much, Dr. Tenforde advises. Former athletes who haven’t run in years may think they can pick up where they left off, but that’s not a smart move — they should also start low and go slow.
For a good couch-to-5K guide, try this beginner’s program from the United Kingdom’s National Health Service.
About the Author

Julie Corliss, Executive Editor, Harvard Heart Letter
Julie Corliss is the executive editor of the Harvard Heart Letter. Before working at Harvard, she was a medical writer and editor at HealthNews, a consumer newsletter affiliated with The New England Journal of Medicine. She … See Full Bio View all posts by Julie Corliss
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD

Prostate cancer: Brachytherapy linked to long-term risk of secondary malignancies

When cancer patients are treated with radiation, it’s possible that the therapy itself may cause new tumors to form in the body later. Radiation kills cancer cells by damaging their DNA, but if the treatments cause genetic damage to normal cells near the radiation target, there’s a small risk that these secondary malignancies may arise over time.
Just over 10 years ago, Canadian researchers set out to assess the risk of secondary malignancy among men with prostate cancer who were treated with a type of radiation called brachytherapy. Unlike radiation delivered from sources outside the body, brachytherapy is accomplished by implanting dozens of radioactive pellets, or “seeds,” directly into the tumor site. Those seeds, which are never removed, emit radiation at a dose that declines toward zero over the course of a year.
Brachytherapy has the advantage of convenience. Instead of traveling for repeat sessions of radiation, men need only one treatment, usually given in an outpatient setting. But brachytherapy is also falling out of favor, in part because newer types of external beam radiation deliver high-precision doses with fewer side effects.
Study methodology and results
The Canadian study compared rates of secondary malignancies in the pelvis among men treated either with brachytherapy or with surgery to remove the prostate. All the treatments took place in British Columbia between 1998 and 2000. The brachytherapy group included 2,418 men with an average age of 66, while the surgically-treated group contained 4,015 men whose average age was 62. Within that group, 2,643 men had been treated with surgery alone, and 1,372 men with surgery plus external beam radiation given later.
After median follow-ups of between 5.8 years (brachytherapy) and 6.4 years (surgery), the study team reported in 2014 that there was no difference in rates of secondary malignancies between the groups, or with cancer incidence in the general population.
But that’s no longer the case: In April 2024, the researchers published updated findings. This time, rates of new cancers in the pelvis — including the bladder and rectum — were higher in the brachytherapy group. Specifically, 6.4% of brachytherapy-treated men had secondary malignancies at 15 years of follow-up, increasing to 9.8% after 20 years. By contrast, 3.2% and 4.2% of surgically-treated men developed secondary pelvic malignancies over the same durations. There was no difference in deaths from secondary malignancies between the groups.
The strength of the association with bladder cancer in particular is “similar to that seen with smoking,” wrote the author of an accompanying editorial. Results from the study “should be considered when treating men with localized prostate cancer who have a long life expectancy,” the authors concluded.
Commentary from experts
“I do believe that this study reveals a dark truth about radiation for prostate cancer that has been long suspected,” says Dr. Anthony Zietman, a professor of radiation oncology at Harvard Medical School and Massachusetts General Hospital, and a member of the advisory and editorial board for the Harvard Medical School Guide to Prostate Diseases. “As the decades pass after radiation therapy of any kind — brachytherapy or external beam — the risk for radiation-induced malignancies rises.
“These malignancies are usually in adjacent organs like the bladder and rectum, or within the prostate itself. They may be very curable, and thus the survival rates are the same for radiation or surgically treated patients, but there is little doubt that, for these patients, they represent a ‘sting in the tail’ long after the radiation has been given and forgotten. This data certainly gives us pause when offering radiation to very young men with several decades of life expectancy ahead of them, and it also reminds us of the value of follow-up visits.”
“The fact that second cancers arise in the area where radiation was given is not surprising, but the magnitude of the long-term increases is concerning,” added Dr. Marc Garnick, the Gorman Brothers Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, and editor in chief of the Harvard Medical School Guide to Prostate Diseases. “There are other common and troublesome urinary side effects of brachytherapy — independent of second cancers — that patients should fully consider before selecting it as a treatment option. This is especially true given the availability of other convenient and similarly effective prostate cancer therapies.”
About the Author

Charlie Schmidt, Editor, Harvard Medical School Annual Report on Prostate Diseases
Charlie Schmidt is an award-winning freelance science writer based in Portland, Maine. In addition to writing for Harvard Health Publishing, Charlie has written for Science magazine, the Journal of the National Cancer Institute, Environmental Health Perspectives, … See Full Bio View all posts by Charlie Schmidt
About the Reviewer
Marc B. Garnick, MD, Editor in Chief, Harvard Medical School Annual Report on Prostate Diseases; Editorial Advisory Board Member, Harvard Health Publishing
Dr. Marc B. Garnick is an internationally renowned expert in medical oncology and urologic cancer. A clinical professor of medicine at Harvard Medical School, he also maintains an active clinical practice at Beth Israel Deaconess Medical … See Full Bio View all posts by Marc B. Garnick, MD

Wildfires: How to cope when smoke affects air quality and health

As wildfires become more frequent due to climate change and drier conditions, more of us and more of our communities are at risk for harm. Here is information to help you prepare and protect yourself and your family.
How does wildfire smoke affect air quality?
Wildfire smoke contributes greatly to poor air quality. Just like fossil fuel pollution from burning coal, oil, and gas, wildfires create hazardous gases and tiny particles of varying sizes (known as particulate matter, or PM10, PM2.5, PM0.1) that are harmful to breathe. Wildfire smoke also contains other toxins that come from burning buildings and chemical storage.
The smoke can travel to distant regions, carried by weather patterns and jet streams.
How does wildfire smoke affect our health?
The small particles in wildfire smoke are the most worrisome to our health. When we breathe them in, these particles can travel deep into the lungs and sometimes into the bloodstream.
The health effects of wildfire smoke include eye irritation, coughing, wheezing, and difficulty breathing. The smoke may also increase risk for respiratory infections like COVID-19. Other possible serious health effects include heart failure, heart attacks, and strokes.
Who needs to be especially careful?
Those most at risk from wildfire smoke include children, older adults, outdoor workers, and anyone who is pregnant or who has heart or lung conditions.
If you have a chronic health condition, talk to your doctor about how the smoke might affect you. Find out what symptoms should prompt medical attention or adjustment of your medications. This is especially important if you have lung problems or heart problems.
What can you do to prepare for wildfire emergencies?
If you live in an area threatened by wildfires, or where heat and dry conditions make them more likely to occur:
- Create an evacuation plan for your family before a wildfire occurs.
- Make sure that you have several days on hand of medications, water, and food that doesn't need to be cooked. This will help if you need to leave suddenly due to a wildfire or another natural disaster.
- Regularly check this fire and smoke map, which shows current wildfire conditions and has links to state advisories.
- Follow alerts from local officials if you are in the region of an active fire.
What steps can you take to lower health risks during poor air quality days?
These six tips can help you stay healthy during wildfire smoke advisories and at other times when air quality is poor:
- Stay aware of air quality. AirNow.gov shares real-time air quality risk category for your area accompanied by activity guidance. When recommended, stay indoors, close doors, windows, and any outdoor air intake vents.
- Consider buying an air purifier. This is also important even when there are no regional wildfires if you live in a building that is in poor condition. See my prior post for tips about pollution and air purifiers. The EPA recommends avoiding air cleaners that generate ozone, which is also a pollutant.
- Understand your HVAC system if you have one. The quality and cleanliness of your filters counts, so choose high-efficiency filters if possible, and replace these as needed. It's also important to know if your system has outdoor air intake vents.
- Avoid creating indoor pollution. That means no smoking, no vacuuming, and no burning of products like candles or incense. Avoid frying foods or using gas stoves, especially if your stove is not well ventilated.
- Make a "clean room." Choose a room with fewer doors and windows. Run an air purifier that is the appropriate size for this room, especially if you are not using central AC to keep cool.
- Minimize outdoor time and wear a mask outside. Again, ensuring that you have several days of medications and food that doesn't need to be cooked will help. If you must go outdoors, minimize time and level of activity. A well-fitted N95 or KN95 mask or P100 respirator can help keep you from breathing in small particles floating in smoky air (note: automatic PDF download).
About the Author

Wynne Armand, MD, Contributor
Dr. Wynne Armand is a physician at Massachusetts General Hospital (MGH), where she provides primary care; an assistant professor in medicine at Harvard Medical School; and associate director of the MGH Center for the Environment and … See Full Bio View all posts by Wynne Armand, MD

A hot weather plan is essential to staying healthy

Here’s a new fact about spring, summer, fall, and sometimes even winter: now that climate change has blurred seasonal boundaries, sizzling heat may be on the way, or currently blanketing your community.
High temperatures stress the body, leading to thousands of heat-related illnesses and deaths every year in the US. Creating a personal heat plan can help you stay safe when the heat index soars.
Caleb Dresser, MD, MPH, is the health care solutions lead for C-CHANGE, the Center for Climate Health and the Global Environment at the Harvard T.H. Chan School of Public Health, and an emergency medicine doctor at Harvard-affiliated Beth Israel Deaconess Medical Center. Below we interview him about who, how, and why heat harms. Then we’ll help you create your personal heat safety plan.
Interview edited for clarity
Who is especially vulnerable during hot weather?
High temperatures can affect anyone. But some people — children, outdoor workers, people who are pregnant or have health problems or disabilities, and older people — are more likely to experience harm when temperatures rise. For example:
- Young children, especially babies, have less physical capacity to deal with very high temperatures.
- People working outdoors may not have access to shade and could be performing physically intensive labor. They need adequate hydration, adequate breaks, and access to a cool space during break time, as OSHA guidelines spell out.
- People with chronic medical conditions, such as kidney disease or heart disease, may have difficulty adapting physiologically to hot weather, or may be more susceptible to its health impacts.
- And some people living with disabilities or certain neurological conditions may have difficulty with thermoregulation — that is, controlling the temperature of their bodies — or may not be able to take actions that keep them safe, such as taking off layers or moving to a cool area.
Which weather patterns create dangerous levels of heat?
Dangerous heat is the result of both high temperatures and high humidity, which interfere with our ability to cool off by sweating. In dry areas, extremely hot temperatures can be dangerous on their own.
Danger zones vary across the United States and around the world. But hospital use and deaths rise once we get above threshold temperatures. The threshold varies in different places depending on whether bodies, cultures, and architecture are adapted to heat.
For example, here in New England, where some people (particularly those of limited means) may not have access to air conditioning, we see increases in healthcare use and deaths at a lower temperature than in the American South, where people and organizations may be more used to dealing with hot weather.
When does hot weather become dangerous to our health?
Risk goes up the longer hot weather sticks around.
One hot day can put some people at risk. A stretch of several hot days in a row during a heat wave is particularly dangerous because it can overwhelm people’s ability to adapt. Eventually people run out of physiological reserves, leading to greater health harms and greater need for medical care.
Surprisingly, spring and early summer are particularly dangerous times because people and organizations aren’t as prepared for hot weather.
How to create your personal heat safety plan
Five key points to help you create a personal heat plan are below. Americares offers further information through heat tip sheets developed with the Harvard C-CHANGE team that are tailored to people in different health circumstances.
Planning is important because intense heat is occurring more often: a Climate Central analysis found 21 additional risky heat days, on average, for 232 out of 249 locations between 1970 and 2022.
- Stay ahead of hot weather. Check apps, websites, TV, or radio for updates on weather today and in coming days. If local weather alerts are available by phone or text, sign up.
- Have a cooling plan. When temperatures soar, you need to spend as much time as possible in cool spaces. Plan options if your home is likely to be too hot and unsafe to stay in. You may be able to stay with a neighbor or family member who has air conditioning until a heat wave passes. Many cities and towns have neighborhood splash pads for children, and open cooling centers or air-conditioned libraries, public buildings, or community centers to everyone — sometimes even overnight. Spending time in air-conditioned businesses or malls, or in a shady green space like a park, may help too.
- Sip plenty of fluids. Water is the best choice. Skip sugary drinks and avoid caffeine or alcohol.
- Use fans correctly. Fans help if surrounding air is relatively cool. If air temperatures are very high, it’s important to dampen your clothes or skin to help keep your body from overheating, and move to a cooler location, if possible.
- Know your personal risks and the signs of heat-related illness. If you have health problems or disabilities, or take certain medicines such as diuretics, talk to your doctor about the best ways for you to cope with heat. It’s also essential to know the signs of heat-related illnesses, which range from heat rash and sunburn to heat cramps, heat exhaustion, and heat stroke. This chart from the Centers for Disease Control and Prevention describes the signs to look for and what you can do, particularly when heat becomes an emergency.
About the Author

Francesca Coltrera, Editor, Harvard Health Blog
Francesca Coltrera is editor of the Harvard Health Blog, and a senior content writer and editor for Harvard Health Publishing. She is an award-winning medical writer and co-author of Living Through Breast Cancer and The Breast … See Full Bio View all posts by Francesca Coltrera
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD